BORN Frequently Asked Questions
This page captures midwives frequently asked questions about data entry into the BORN Information System (BIS).
The responses to these questions reflect the collective consensus of the AOM-BORN Knowledge Translation Task Force and were approved by BORN staff. This Task Force recommended changes to the BIS to increase the ease at which midwives may enter data about their clients without error or confusion, while also advancing the quality and relevance of midwifery-specific data.
Questions about consultations and transfers of care? Visit our Consultations and Transfers of Care webpage with a specific FAQ for this topic.
This page is monitored and updated as the BIS continues to improve. Midwives are welcome to submit additional concerns related to the BIS and BIS data elements to AOM staff to this email: research@aom.on.ca.
Review the Frequently Asked Questions below or search for your specific question.
General BIS Questions
Changes to BORN haven’t been implemented in my hospital yet. What should I enter?
The implementation of BORN enhancements will be delayed in approximately 14 Ontario hospitals beyond the May 1st 2024 go live date, and into the fall. Since midwifery enhancements are automatic, until their hospital goes live, midwives at the affected sites have two options:
1. Enter 'unknown' for these new data elements in the encounters, when logged in under the midwifery practice group → Submit
OR
2. Using the checklist here, enter the data for the clients under the midwifery practice group → Submit
Where can I find a breakdown of the recent midwifery-relevant changes to the BIS?
The midwifery-relevant changes to the BIS can be found on this page of the AOM website (login required) under "Enhancements to the BIS".
Many of these new changes were recommended by the BORN-AOM Knowledge Translation Task Force, a group of midwives with expertise in or experience with the BIS. These improvements aim to increase the ease at which midwives can enter data about their clients without error or confusion, while also advancing the quality and relevance of midwifery-specific data.
[March 13, 2024]
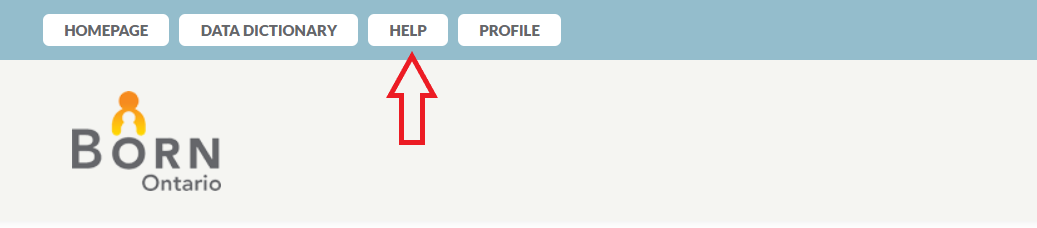
Where can I find help in the BIS?
If you have a question about a specific data element, first examine what is written in "label help". Label help can be accessed in the BIS for every data element. Simply hover over and click on the data element in question and a box will appear providing more information about that data. This help will include the definition of the data element, but may also include more information about each pick-list option and when they should be selected.
Below are examples of label help available in the BIS for two different data elements.
If you require general help or wish to access BORN's many training materials, navigate to the top left hand corner of the screen and click on the "Help" button. Here you will find contact information for the BORN Helpdesk, Archived Training Materials, the BIS Enhancement Request Form and BORN Training and Reference Materials.
BORN also provides additional midwifery-specific resources on their website here.
You may also find the answer you seek on this FAQ page. Use the search bar above to see if your question has already been addressed. If not, you may request that your question is added to this page by emailing: research@aom.on.ca
If you require immediate assistance, you may reach out to your respective Regional BORN Coordinator via email or call the BIS help desk toll-free at 1-855-881-BORN (2676) and they will be happy to help you with your specific concern.
I frequently see empty data fields in the BIS that should have been recorded by a hospital staff member and prepopulated for me. Why is this the case?
When encountering empty data fields in the BIS, enter the most complete and accurate information available. If no information is available, it is appropriate to select unknown.
Empty fields will appear in the BIS if:
- A hospital staff member has indicated “unknown” for that field. BORN has an algorithm in place that will not allow "unknown" to prepopulate for midwives. This is BORN's attempt to collect the most complete data, hoping that the midwife will be able to provide known data.
- Data has been entered by hospital staff but has not yet prepopulated. In some cases, there may be a delay in the upload of data into the BIS.
- Data has not yet been uploaded into the BIS by the hospital.
- If a midwife opens up an encounter under their MPG before hospital BORN data was entered and submitted, the data will not pre-populate from the hospital to the midwifery practice group data. The order of data entry is important. Hospital organizational data first, then midwifery practice group organizational data second.
To ensure that critical BORN data is collected by midwives during the labour and birth, the AOM has created a Labour & Birth BORN Data Template. Midwives may find this tool useful to keep track of data that is not captured in other existing client records.
Why do yellow and red alerts sometimes appear when I try to proceed with data entry?
Red and yellow alerts in the BIS are designed to assist the user in entering accurate data.
A red alert (i.e. Data Element Error) will prevent a user from proceeding until the error in data entry is corrected. The midwife will not be able to continue entering data into the BIS without changing the data entered when a red alert is encountered.
A yellow alert (i.e. Data Element Quality Check) is a warning to a user to indicate that a possible error may have occurred. When a yellow alert appears, review the indicated data entry for accuracy. If inaccurate, correct the data entry. If accurate, disregard the warning and proceed. The midwife can continue to enter data without changing their data entry if a yellow alert is encountered.
The AOM has worked with BORN to improve clarity in the language used in the red and yellow alerts. The following screen shots display examples of how a red and yellow alert will appear in the BIS:
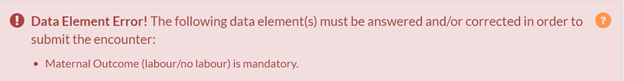
If a midwife is having trouble submitting an encounter, they are welcome to contact their respective BORN Regional Coordinator to resolve their concern.
Antenatal General Encounter
My MPG does not routinely record the weight of our clients. How can I indicate this in BORN?
BORN has included the option for “declined weight check” into the BIS. This option can be selected for clients who have indicated that they do not wish to record their weight.
However, if the weight of a client is not known because it was not asked by a midwife, “unknown” should be selected.
Midwives should make every effort to record the most complete data when possible. When discussing weight, comments should involve the sensitive use of language and should be clear and carefully explained within the context of the client’s unique clinical picture.
For more information on how low or high body mass index (BMI) may influence pregnancy and for tips on how to have respectful and constructive informed choice conversations with clients about BMI, please see the AOM’s Clinical Practice Guideline: The Management of High or Low Body Mass Index during Pregnancy, updated in 2019.
My client experienced a pregnancy loss under 20 weeks gestation. Do I need to complete BORN data entry?
It is highly encouraged that you enter this client’s data into the BIS. This data can be used to examine how much care midwives have provided before pregnancy loss and have continued to provide to their clients after pregnancy loss.
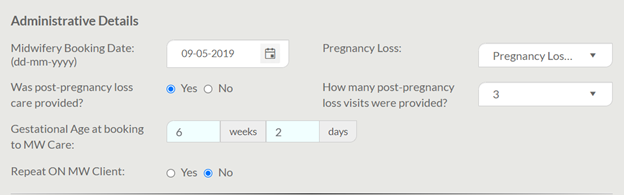
The Midwifery tab in the Antenatal General encounter allows midwives to capture post-pregnancy loss follow-up visits. This data element is located at the bottom of the Midwifery tab under “Administrative Details”.
If pregnancy loss under 20 weeks is selected, a new data element will appear asking “Was post-pregnancy care provided?”. If yes, the user may select how many visits were provided. Importantly, “visits” includes each in-person, virtual, and phone visit as separate visits.
The below screen shot demonstrates a hypothetical example of how data entry for a pregnancy loss under 20 weeks could appear in the BIS.
Is there a way to automatically count how many visits occurred with each midwife and at each location?
Unfortunately, there is no universal way to automatically count how many visits a client has had with each midwife and at each location. This is because MPGs across the province have different methods for recording their client information; some use EMRs and some do not. If you practice uses an EMR, you may find this information within the appointment history for your client.
The BIS asks midwives for this important information because it can be used to identify continuity of care. This data can be pulled from the BIS and used by midwifery researchers for advocacy and policy change purposes.
If my senior student conducted some clients visits alone during the antenatal period, do I add those visits under me (coordinating midwife) in the Clinical & Visits Summary in the Midwifery tab?
Yes. Midwives should be recording each clinical visit their client receives even if only the senior student met with the client. This visit should be recorded under the midwife that is supervising the senior student.
Who qualifies as a maternal antenatal health care provider and should be selected for in the “Antenatal Health Care Provider” data element other than myself (midwife)?
The “Antenatal Health Care Provider” data element asks the user to indicate the designation of all health care providers that provided any antenatal care during the current pregnancy. This is a multi-select field. If care was received from a registered midwife or an aboriginal midwife, select “midwife”.
Selecting care providers other than yourself as the midwife is helpful for BORN to get a sense of the entirely of a client’s antenatal care. There are other ways that midwives are recognized in the BIS as a client’s primary health care provider.
Importantly, this data element is not intended to capture any healthcare provider that the client happens to interact with during the antenatal period but is specific to health care providers that have provided antenatal care. For example, a visit to a chiropractor for back pain or a visit to a family doctor to check-up on asthma would not be included as valid health care providers that apply to this field.
Why does the BIS ask if a client resides with a smoker?
The BIS asks its users to indicate if their client resides with a smoker at the time of the first prenatal visit and at the time of labour/admission. These data elements can be found in both the Antenatal General encounter and the Labour & Birth encounter.
This data element was likely created as a prompt for hospital staff to provide clients with information related to the risks of smoke exposure for newborns and pregnant people. Quantifying second-hand smoke exposure is not the intention behind this question.
When completing data entry for this data element, simply indicate whether a smoker resides in the home, regardless of where the smoking is done.
Labour & Birth Encounter
Why has BORN standardized the definitions of induction and augmentation of labour?
Inconsistent definitions have created discrepancies in documentations and impacts data accuracy. Consistent terminology for induction and augmentation of labour will improve data quality and standardization for quality assurance and improvement.
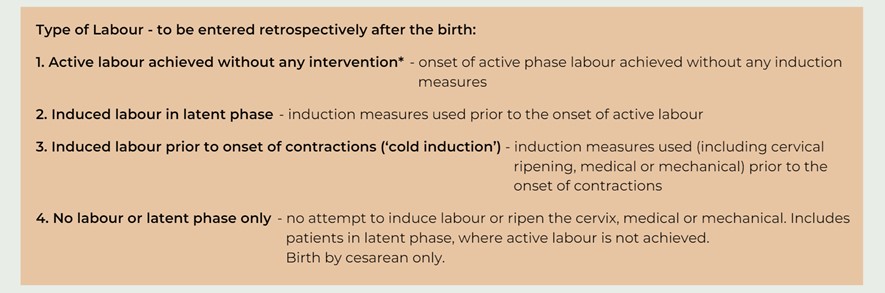
Induction of labour now captures interventions that occur prior to the onset of active labour while augmentation now captures interventions that occur after the onset of active labour. Induction is broken down into “cold induction” and “induction of labour in latent phase of labour”.
Active labour is defined at the presence of regular contractions leading to cervical effacement and dilation at 4 cm or greater in a nulliparous person, or 4 to 5 cm dilation in a multiparous person. Latent labour is a period, not necessarily continuous, when there are contractions and some cervical change, including cervical effacement and dilation up to 3 cm.
The following algorithm organizes how to capture the various scenarios that may arise in labour.
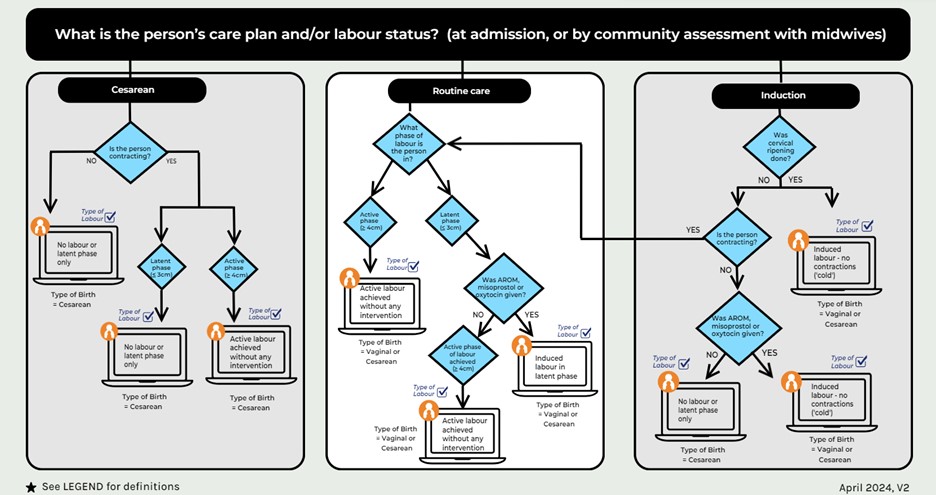
The following table describes the updated definitions for the types of labour that may be selected.
My client had a home or clinic birth. How do I indicate how long I stayed as a midwife?
Four new data elements now record the length of stay of a home or clinic birth, by asking when the first midwife enters a client’s home/clinic to attend to a labour and birth to stay, and when the last midwife has left the home/clinic after the birth. To match data entry in hospital births, midwives will also be asked to report cervical dilation at home.
Data elements to capture length of stay for home births include:
- Time of first midwife’s arrival to home to attend labour and birth
- Date of first midwife's arrival to home to attend labour and birth
- Time of last midwife’s departure from the home following birth
- Date of last midwife’s departure from the home following birth
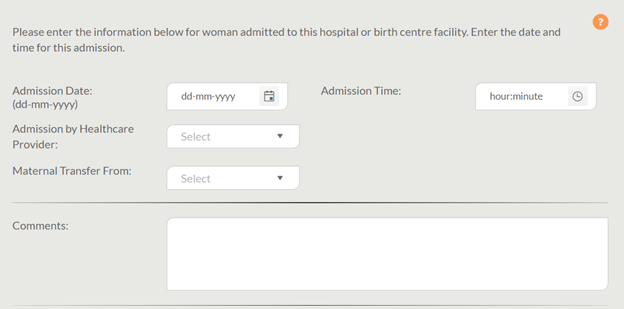
Do admission data elements need to be completed for home or clinic births?
No, admission data elements including “Admission Time”, “Admission Date”, “Admission by Healthcare Provider” and “Maternal Transfer from” should not be completed for home or clinic births. These data elements are for facility births only. Midwives may leave these irrelevant admission data elements blank for a home or clinic birth where no transfer to hospital occurred.
Below is a screen shot of the BIS displaying the Admission Tab in the Labour & Birth Encounter where the admission data elements not relevant to a home birth appear. Note that the text at the top indicates specifically that this information is for a client admitted to a hospital or birth centre facility only.
What information should be inputted into the “ID of Healthcare Provider Attending Birth” field?
This is an optional data element that was created to support the needs of individual organizations or MPGs. Midwives may choose to leave this field blank.
If the data element “ID of Healthcare Provider Attending Birth” is hovered over and clicked, the following label help box will appear:
The identification of the most responsible person attending the birth can be entered into this field, if desired. However, exactly which type of identification is entered is up to the user’s discretion. Some organizations input an anonymous numeric code, other input the initials of the healthcare provider. The code entered in this field can consist of letters, numbers, or a combination of both.
MPGs that choose to enter data in this field can use it however they see fit. That is, data can be entered using free text, such as names, but also numerical data such as registration numbers, up to 50 characters. If this information is not known, the field can be left blank. Some examples include:
- entering midwives’ initials when multiple midwives have provided care during labour; or
- entering OB initials to keep track of transfers of care
Once I indicate that my client was induced, I am no longer given the option to fill out augmentation information. Why is this the case?
The 2024 BIS Enhancements remedy this previous issue. The BIS now asks midwives to report “Type of labour” data element (“active labour without intervention” or “induced - cold or “induced - latent” or “latent/no labour”) and all the following data elements are visible for data entry (i.e. cervical ripening/induction methods, date/time of oxytocin, date/time and type of membrane rupture, and date/time of the stages and phases of labour.) The BIS will validate inductions and augmentations in the backend from this objective data.
For the purposes of BORN data collection, induction of labour refers to an intervention(s) that occur prior to the onset of active labour to ripen the cervix and/or initiate the process of labour by artificial means, involving the use of: prostaglandins, misoprostol, mechanical/foley catheter, or laminaria tents.
Prostaglandin used for cervical ripening may be enough to induce labour with no further interventions. How do I record this information correctly? Is this considered an induced labour?
Yes, this would be considered an induced labour. For this specific scenario where prostaglandins are the only intervention of cervical ripening and no other method of induction was used, the following options should also be selected:
- Method of Induction/Cervical ripening – Prostaglandin
- Type of labour – Induced, no contractions; or, induced in latent phase
In some circumstances, the “time started pushing” precedes “time fully dilated”. When I indicate this in the BIS, a yellow alert box appears. Am I able to proceed with this data entry as is?
When the “time started pushing” precedes “time fully dilated”, you will encounter a yellow ‘data element quality check’ alert box: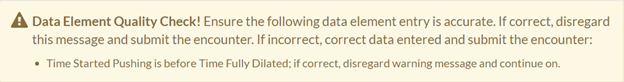
This alert is intended to assist a user who may have accidently entered data incorrectly, as pushing does not precede full dilation in the majority of cases. This alert will not prevent you from indicating the correct series of events.
When a yellow alert appears, review the data you have entered to ensure accuracy and then, if accurate, disregard the warning and proceed with data entry.
My client had a planned hospital birth but laboured at home for some time. When the “Maternal transfer from” data element was completed by hospital staff, the staff person incorrectly selected the “Home birth/MW care” option. How can I prevent this from happening?
The option “Home birth/MW care” for the “Maternal transfer from” data element has been removed during this update. The following options are now available for the “Maternal transfer from” data element:
- No transfer
- Hospital – Name
- Planned Home or Clinic Birth
- Nursing Station
- Birth Centre
- Other unit, same hospital
- Other
For a client that has planned for a hospital birth before the onset of any labour, the option “No transfer” should be selected. This is true even if a client was planning a home/birth centre/clinic birth during pregnancy but changed their plan to a hospital birth before the onset of any labour.
If a client planned a home/birth centre/clinic birth up to and including any labour but decided during labour to be transferred to the hospital, the correct pick list option to select would be “Planned Home or Clinic Birth” or “Birth Centre”, depending on the client’s plan.
For more information on which pick-list option to select, a user may check the field level help in the BIS by hovering over and clicking the data element of concern. A help box should appear with more information.
Postpartum Maternal Encounter
Do discharge data elements need to be completed when my client has given birth at home and was not transferred to the hospital?
When “Birth location” is indicated as “home” in the BIS, the BIS will automatically remove two irrelevant data elements in the Postpartum Child and the Postpartum Maternal encounters: “Discharge weight” and “Newborn feeding from birth to discharge”.
For the BIS to remove other irrelevant discharge data elements, the following actions must be made:
- “No transfer” must be selected when asked “Maternal outcome” in the Postpartum Maternal Summary tab; and
- “No transfer” must be selected when asked “Newborn discharged or transferred to” in the Postpartum Child Discharge Summary tab.
By selecting “No transfer” in both encounters, discharge date and discharge time will not appear, and this information will not need to be entered.
Locating the “Newborn Discharged or Transferred to” and “Maternal Outcome” Data Elements
The screenshot below demonstrates where the “Newborn discharged or transferred to” data element is located in the Postpartum Child encounter under the “Discharge Summary” tab with the correct response selected:
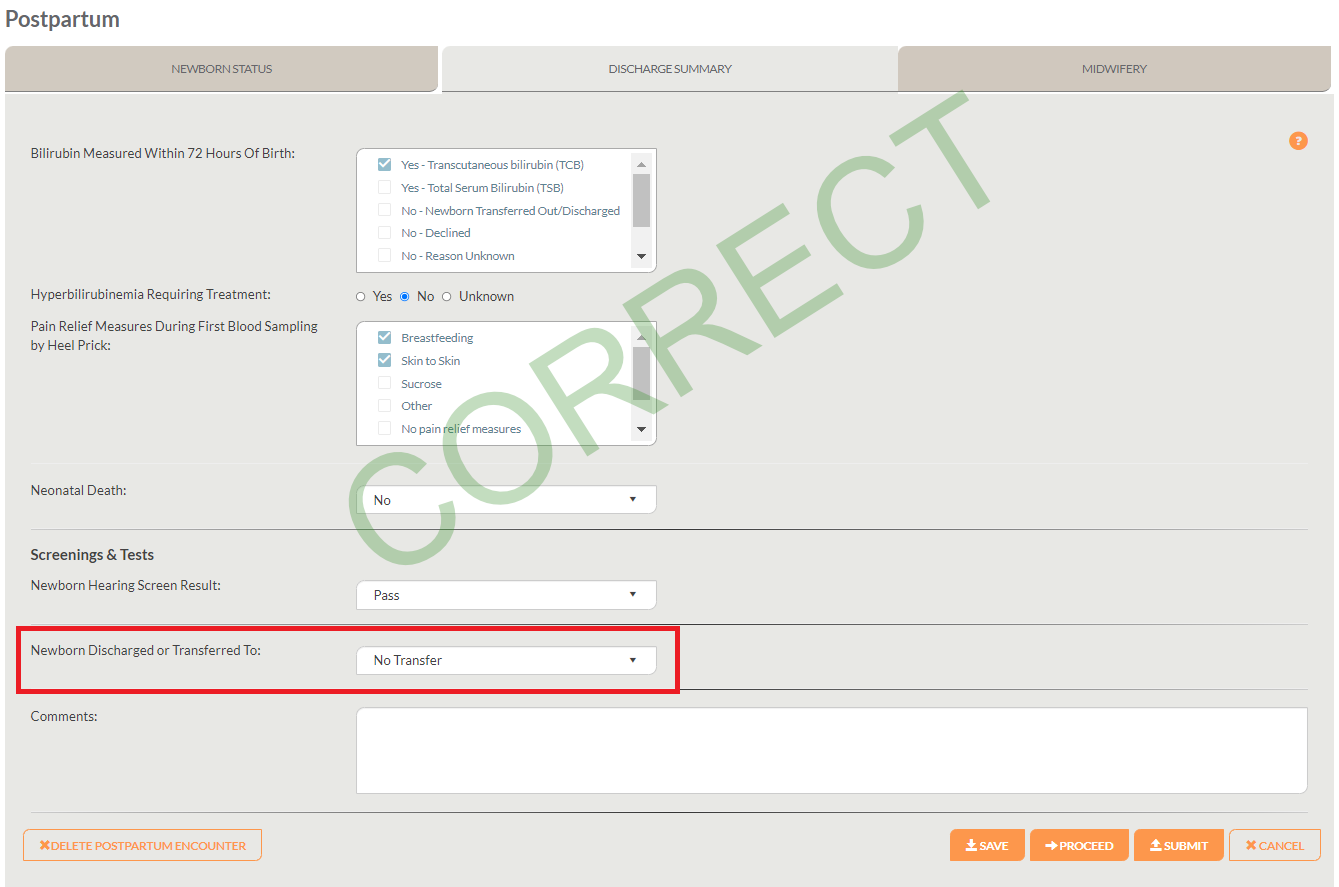
Although it may be tempting to select “Home” when a client has had a home birth, this is incorrect and would require forced data entry for discharge time and date, which are irrelevant to home births with no transfer to hospital. This remains the same so as to capture clients that may be transferred to the hospital during or immediately following a home birth. Below, the screen shot demonstrates how new data elements appear when “Home” is selected for “Newborn Discharged or Transferred to”:
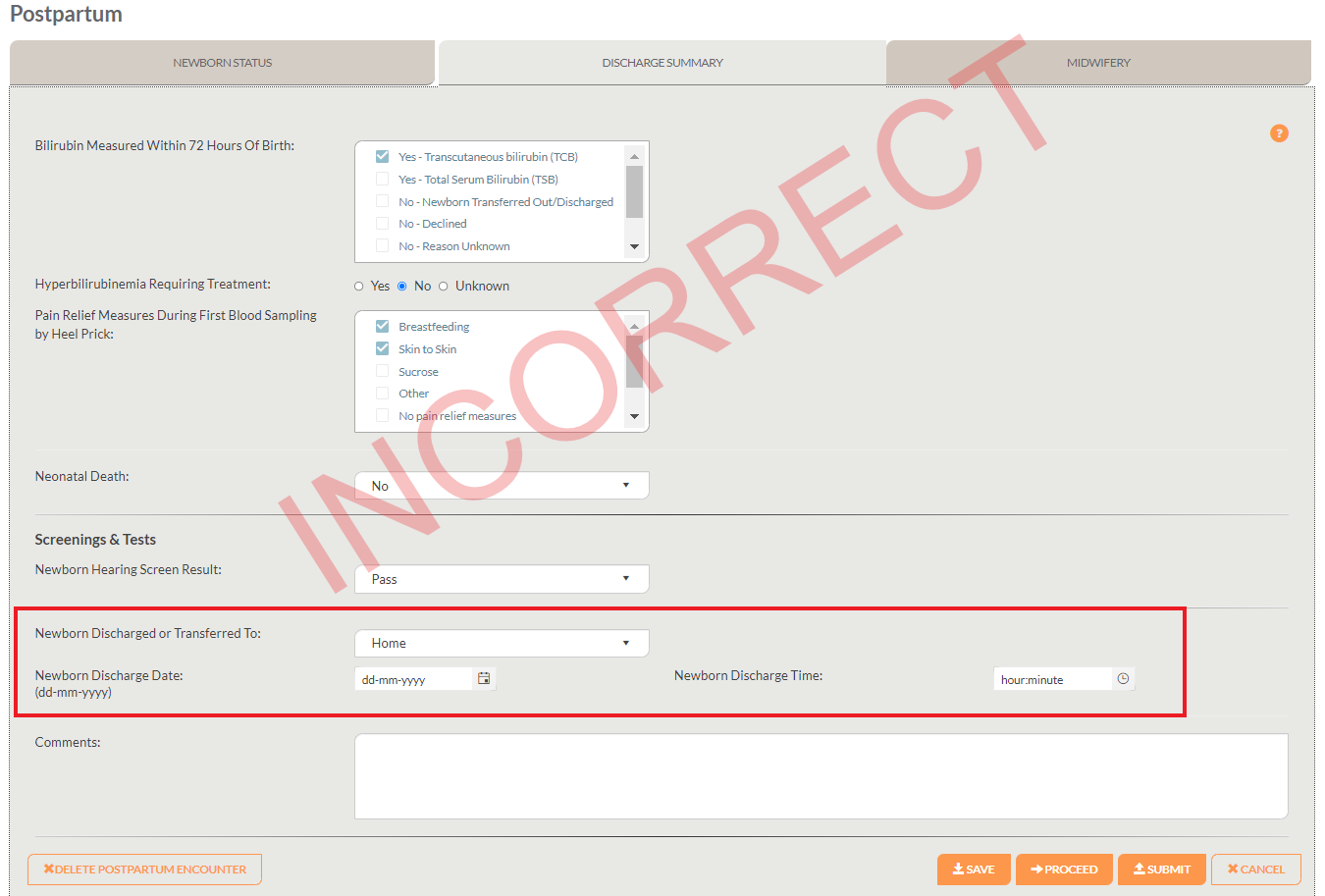
Additionally, this below screen shot indicates where the “Maternal outcome” data element is located in the Postpartum Maternal encounter under “Summary” with the correct response selected:
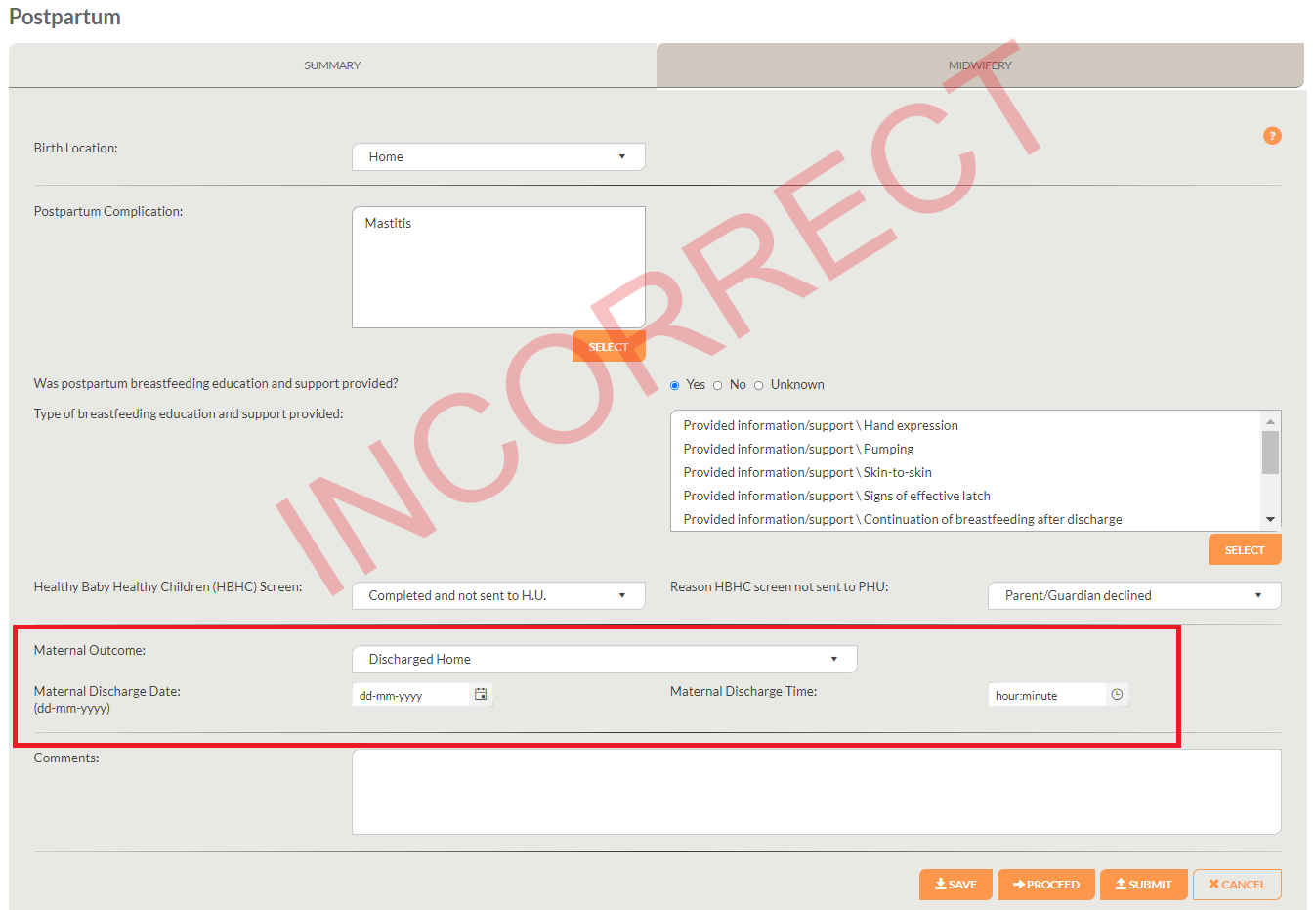
Similarly, new data elements will appear asking for discharge date and time if the response “Discharged home” is incorrectly selected for this data element:
When a client declines Healthy Baby Healthy Children (HBHC) screening, how do I enter this in the BIS?
It is important to properly indicate when the HBHC screen has been declined by a client because this ensures that the screen is not registered as missing or incomplete.
Entering a declined HBHC screen in the Postpartum Maternal encounter is a two-step process. See the steps below:
- For the data element “Healthy Baby Healthy Children (HBHC) Screen”, indicate: “Not completed.”
- A new data element should appear titled “Reason HBHC screen not sent to PHU”, for this field indicate: “Parent/Guardian declined”.
The screenshot below displays how these two data elements will appear in the BIS.
The HBHC encounter will pre-populate with all relevant information that has already been entered, saved and submitted in the BIS. Even when a client declines the HBHC screen, an HBHC encounter should still be created for this client. To access midwifery-specific resources on how to use the HBHC encounter, see this page on the AOM website (login required).
To indicate that a client has declined the HBHC screen in the HBHC encounter, create and open the HBHC encounter. At the top of the HBHC encounter under the “Consent and Demographics” tab, indicate “No” for the question “Client consents to share personal information and personal health information have been obtained”. The below screen shot displays where this question appears on the HBHC encounter.
Once “No” is selected, indicate the consent method and the reason for consent declined. The encounter can then be saved and submitted without completing the rest of the “Consent and Demographics” tab or the “Questionnaire” tab.
Postpartum Child Encounter
I select “unknown” for the data element “Pain Relief During First Blood Sampling” when the newborn blood sample is drawn by a nurse. Is this appropriate?
If you are unaware of the pain relief method and you are met with an empty field for this data element when completing data entry, selecting “unknown” is appropriate.
Nurses who complete the first blood sampling in hospital should be inputting this information into BORN and this field should be prepopulated when a midwife signs into the BIS. However, this may not always be the case. If a nurse indicated “unknown” for this field, “unknown” will not be pre-populated, and a midwife will later see an empty field in which information is required. Additionally, it can take some time for hospital data to pre-populate for midwives.
If this data is not being inputted by the nurses at the hospital, some MPGs have been successful at writing orders requesting nurses to complete this information in BORN.
Why is there no option to indicate that visual assessment was done to assess for jaundice?
The BIS does not directly ask how a healthcare provider assessed a newborn for jaundice. Rather, the BIS asks if bilirubin was measured within 72 hours of birth. For this data element, the pick-list options are as follows:
- Yes - Transcutaneous bilirubin (TCB)
- Yes - Total Serum Bilirubin (TSB)
- No - Newborn Transferred Out/Discharged
- No – Declined
- No – Reason Unknown
- No – Reason other
- Unknown
If bilirubin was not measured before the baby was discharged from the hospital but returns for testing within 72 hours, select No – Newborn Transferred Out/Discharged/
If TCB and TSB were both performed, select both.
The AOM acknowledges that midwives and/or clients following an informed choice discussion may choose to not conduct a TCB or TSB test for low-risk newborns after visual assessment. If bilirubin was not measured with a TCB or TSB test due to midwife discretion, “No – Reason Other” should be selected. If bilirubin was not measured with a TCB or TSB test due to client choice, "No - Declined" should be selected.
Guidance related to visual assessment and bilirubin measurement in the newborn are available in the AOM’s Clinical Practice Guideline on Hyperbilirubinemia.
How do I complete this data entry for the Newborn Hearing Screen if I do not have the result?
The Newborn Hearing Screen should be conducted before a client is discharged from the hospital in the postpartum, or within the first two months after birth in the community. The “Newborn Hearing Screening Result” data element has recently been updated as of April 2021 to include new pick list options. A BIS user can now indicate one of the following pick-list options:
- Pass
- Referral
- Inconclusive/no result
- Referred to community
- Not done
- Unknown
As the primary care provider, you should have access to the result of the newborn hearing screen. However, in some cases the screen result is not provided directly to the midwife and may only be provided to the client. It may be useful to check in with the client to find out the result of the screen. If after checking with the client the result remains unknown, you may select "unknown".
IMPORTANT: When entering data for this data element, midwives should always assume that the BIS wants the most current Newborn Hearing Screen Result, which may be up to 6 weeks PP for midwifery clients, not just ‘discharge’ results from hospital births.
The following table indicates the correct selection for the “Newborn Hearing Screen Result” based on specific scenarios:
|
pICK-LIST OPTION |
Appropriate Scenario(s) |
|
Pass |
Select if:
|
|
Referral |
Select if:
|
|
Inconclusive/no result |
Select if:
|
|
Referred to community |
Select if:
OR
|
|
Not done |
Select if:
|
|
Unknown |
Select if:
OR
|
When is it appropriate to indicate the same weight for both the birth weight and the discharge weight for a newborn?
It is common for midwifery clients that give birth in the hospital or a birth centre to be discharged in less than 24 hours after a birth. In some cases, the newborn weight may be collected directly after the birth only, and no additional weight is taken at discharge. Midwives who only have the birth weight and no additional discharge weight may indicate the same weight for both the birth weight and the discharge weight. In the case that a midwife does have a discharge weight, that weight should be entered in the discharge weight field.
For midwifery clients that stay on the postpartum floor with nursing care after the midwife leaves, a discharge weight may be obtained by the nursing staff before the client is discharged. In such cases, the nurse should input the discharge weight into the BIS and this information should pre-populate for the midwife. The midwife would not be required to enter the discharge weight field.
Clients that gave birth at home and were not transferred to the hospital at any time during labour or birth are not formally “discharged” from any facility. For these clients, the "discharge weight" data element should not appear if previous data has been entered correctly. See the above FAQ response for "Do discharge data elements need to be completed when my client has given birth at home and was not transferred to the hospital?" for steps on how to ensure the "discharge weight" data element does not appear in the BIS for a client that has given birth at home.