Consultations & Transfers of Care in BORN
Recording Consultations & Transfers of Care in the BIS Infographic (PDF, 490 KB) (Published July 2022)
Recording consultations and transfers of care (TOC) in the BORN Information System (BIS) can be challenging. Below is a segment of our new infographic that provides our top tips and reminders. Click on the image to view the full infographic (PDF, 490 KB) or click the link above.
View Recording Consultations & Transfers of Care in the BIS infographic transcript.
Consultations & Transfers of Care FAQ
More questions about consultations and TOC? We have answers! Review the FAQs below or search for your specific question. Midwives are welcome to request new questions to be added to our FAQ by emailing research@aom.on.ca.
Where to Record a Consultation/TOC
Where do I record a consultation/TOC in the BIS?
Every encounter in the BIS has a specific time-period associated with it. Consultations/TOC should be organized based on the time in which they occurred. The BIS time periods are as follows:
- Antenatal General: During pregnancy including early labour, prior to active labour.
- Labour & Birth: From onset of active labour to approximately 1-hour post-birth.
- Postpartum Maternal: Approximately 1-hour post-birth to discharge from midwifery care.
- Birth Child: Within approximately the first hour of birth.
- Postpartum Child: From approximately 1-hour post-birth to discharge from midwifery care.
Take care to not duplicate the same consultation/TOC across multiple encounters.
If you are not sure which encounter/time-period your consultation/TOC falls under, choose the encounter in which the clinical indication that necessitated the consultation/TOC occurred. For example, a PPH that occurred within the first hour after birth, but circumstances arose that delayed the consultation/TOC until 2 hours postpartum should still be recorded in the Labour & Birth encounter.
Induction/Cervical Ripening
Induction of labour and cervical ripening related consultations/TOC are exceptions to the time periods. Although induction and cervical ripening occur before active labour begins, they are integral to the process of labour and birth and therefore consultations/TOC related to induction and/or cervical ripening should be recorded in the Labour & Birth encounter. To learn more about this exception, review the below response to “Where do I record a consultation/TOC related to induction of labour and/or cervical ripening in the BIS?”.
Where do I record a consultation/TOC related to induction of labour and/or cervical ripening in the BIS?
Induction or cervical ripening related consultations/TOC are an exception to the defined time periods for BIS encounters. Although induction and cervical ripening occur before active labour begins, they are integral to the process of labour and birth and therefore consultations/TOC related to induction and/or cervical ripening should be recorded in the Labour & Birth encounter.
There are several reasons for this exception including:
- A client receiving an induction is prepared for imminent active labour and thus induction is a component of the labour & birth experience.
- Induction related data is collected only in the Labour & Birth encounter, and thus data on consultations/TOC should be consistent with the data that has already been entered in the encounter.
When selecting the reason for a consultation/TOC related to induction the primary clinical indication that necessitated the induction should be selected, for example select pre-labour rupture of membranes (PROM) or postdates (≥41 weeks). There is no option in the BIS to select “induction” or "cervical ripening" as the reason for the consultation/TOC.
Where do I record a consultation/TOC related to PPROM or PROM in the BIS?
The encounter in which consultation/TOC data is recorded related to PPROM or PROM would depend on whether labour is initiated directly after the rupture of membranes.
For preterm pre-labour rupture of membranes (PPROM), these consultations/TOC should be recorded in the Antenatal General encounter since they occur before active labour and typically do not result in imminent labour and birth.
Consultations/TOC related to PROM may be recorded in the Antenatal General encounter if PROM does not result in immediate progress toward labour (ex. Induction).
For clients where PROM is used as the clinical indication to justify induction of labour and a consultation/TOC is required to perform this induction, this consultation/TOC should be recorded in the Labour & Birth encounter.
Selecting a Reason for a Consultation/TOC
What do I select as the reason for a consultation/TOC in the BIS?
When selecting the reason for a consultation/TOC, always select the clinical indication or medical condition that justified the need for a consultation/TOC.
Do not select the clinical intervention that occurred after the consultation/TOC.
For example, a consultation for abnormal fetal heart rate may ultimately result in a TOC and a cesarean section, but the reason for this consultation/TOC is based on the original clinical indication (i.e., abnormal fetal heart rate) not the resulting intervention to manage the complication. This is because the trajectory of the client’s care was not certain when the need for a consultation/TOC was determined, and indeed a different intervention (or no intervention) could have been used depending on the clinical circumstances and the physician’s discretion. Additionally, the fact that the client had a cesarean section is captured elsewhere in the BIS (like all other clinical interventions) and does not need to be duplicated in this section.
See the below snippet of our consultations and transfers of care infographic for examples on what to select.
Footnote 3: The examples displayed here will not be applicable to all midwives. Scope of practice may vary; midwives should assess their own knowledge, skills, and judgement to determine when it is appropriate to consult or transfer care.
Should I select multiple reasons for a consultation/TOC?
It is best practice to select a single primary reason for a consultation/TOC. However, if there was another reason that was crucial to necessitate a consultation/TOC, this may be selected as well. Midwives should avoid selecting more than two reasons for a consultation/TOC.
As a reminder, midwives should select clinical indications/complications as the reason for a consultation/TOC, not clinical interventions. For more information visit the above response to the question: “What do I select as the reason for a consultation/TOC in the BIS?”.
It is important to keep in mind the many details of a client’s clinical scenario should already be captured in other areas of the BIS and therefore do not need to be listed in detail in the midwifery tab as reasons for consultations/TOC.
The available list of reasons for a consultation/TOC in the BIS does not include my client’s specific case. How do I record this properly?
As of November 2022, BORN has included a search bar within the reasons for consultations/TOC sections in both the Antenatal General and Labour and Birth encounters. This change was recommended by the AOM and we are very excited to see it be added to the BIS ahead of schedule. This search bar will allow midwives to quickly find the reason for a consultation/TOC without having to scroll the entire list.
If after searching your find that the option you are looking for does not exist, select the most appropriate “other” option. There are many specific “other” options within the drop-down lists of both the Antenatal General and Labour & Birth encounters. The more specific the data entered in the BIS, the better quality it will be. Always attempt to select the most specific “other” if available. For example, if your client has a mental health concern that required a consultation/TOC during pregnancy, but this concern is not listed as an option in the BIS, select “Mental Health Concerns – Other” as the reason for the consultation/TOC in the Antenatal General encounter.
The BIS contains several “other” options that fall within specific categories of complications. The below table lists all the “other” options that are available in each encounter in the order they appear.
|
Encounter |
Specific Other Options |
General Other Options |
|
Antenatal General |
|
|
|
Labour & Birth |
|
|
|
Postpartum Mother |
None. |
|
|
Birth Child |
|
|
|
Postpartum Child |
|
|
When to Record a Consultation/TOC
Midwives at my MPG manage induction of labour/augmentation with oxytocin for our clients and our hospital allows this. Do we need to record this as a consultation in the BIS?
Midwives do not need to record a consultation for an induction of labour/cervical ripening/augmentation if all three of the below conditions are met:
- The midwife has the knowledge, skills, and judgment to manage the induction/cervical ripening/augmentation.
- Hospital protocol does not require that a physician is involved for a midwife to access or manage an induction/cervical ripening/augmentation.
- No physician was consulted with to access the materials required for induction/cervical ripening/augmentation or during the management of an induction/cervical ripening/augmentation procedure; the care was managed solely by the midwife.
If one of more of the above criteria are not met, a midwife should be consulting with a physician and recording this in the BIS. See the above question “Where do I record a consultation/TOC related to induction of labour and/or cervical ripening in the BIS?” for more specific details on how to record this in the BIS.
If a physician attends my client’s labour and/or birth because of a potential birth complication but no complications occur, do I still record this as a consultation/TOC in the BIS?
Depending on the physician’s involvement, this scenario may need to be recorded in the BIS. For example, if a physician may be called to attend a midwifery client’s labour and birth after an abnormal fetal heart rate (FHR) is detected. Below we review three possible series of events related to this example.
- Birth complication -> Atypical/abnormal FHR -> Pediatrician attends birth -> Neonatal indication for consult? -> NO because baby is born vigorous -> Pediatrician does not perform any care and leaves to allow midwife to continue care.
Conclusion: No consultation is recorded in the BIS because the pediatrician did not provide any care. - Birth complication -> Atypical/abnormal FHR -> Pediatrician attends birth -> Neonatal indication for consult? -> NO because baby is born vigorous -> Pediatrician provides care even though it was not clinically indicated, midwife remains most responsible provider (MRP).
Conclusion: A consultation is recorded, although it was not clinically indicated. See below for further explanation on how to record this consultation. - Birth complication -> Atypical/abnormal FHR -> Pediatrician attends birth -> Neonatal indication for consult? -> YES because baby is born requiring care-> Pediatrician provides care as indicated and midwife remains MRP or MRP status is transferred to the pediatrician depending on the clinical scenario.
Conclusion: A consultation or a TOC was clinically indicated and is recorded in the BIS. Select the relevant clinical indication that necessitated the pediatrician’s care.
In BORN we want to do our best to capture every time a physician is involved in a midwifery client’s care if the care provided is relevant to the pregnancy. In scenario #2, the pediatrician was involved in some care after the birth. However, it was not necessary that this care was provided by the pediatrician since no clinical complication occurred and the midwife would have been able to adequately provide this care themselves. To capture that the physician was involved in the care, a consultation should be entered into BORN with “Other, specify” selected as the reason for the consultation. The following actions should occur to record this consultation correctly:
- An Infant consultation/transfer of care is entered.
- “Other, specify:” is selected as the infant condition, along with manually entering a brief description the describes the scenario ex. “pediatrician called to birth”
- Select “Yes” for “Infant consultation(s) with a Physician”
- Select “Yes” for “Was rationale for consult due to hospital/physician protocol?’
- Select “No” for “Infant Transfer of Care”.
- Select “No” for “Infant Outpatient (+Emergency) Hospital Services”.
It’s important to note that this scenario would NOT be considered a transfer of care since the midwife remained the MRP even as the physician provided care.
The below screen shot provides a visual of the data inputted for scenario #2:
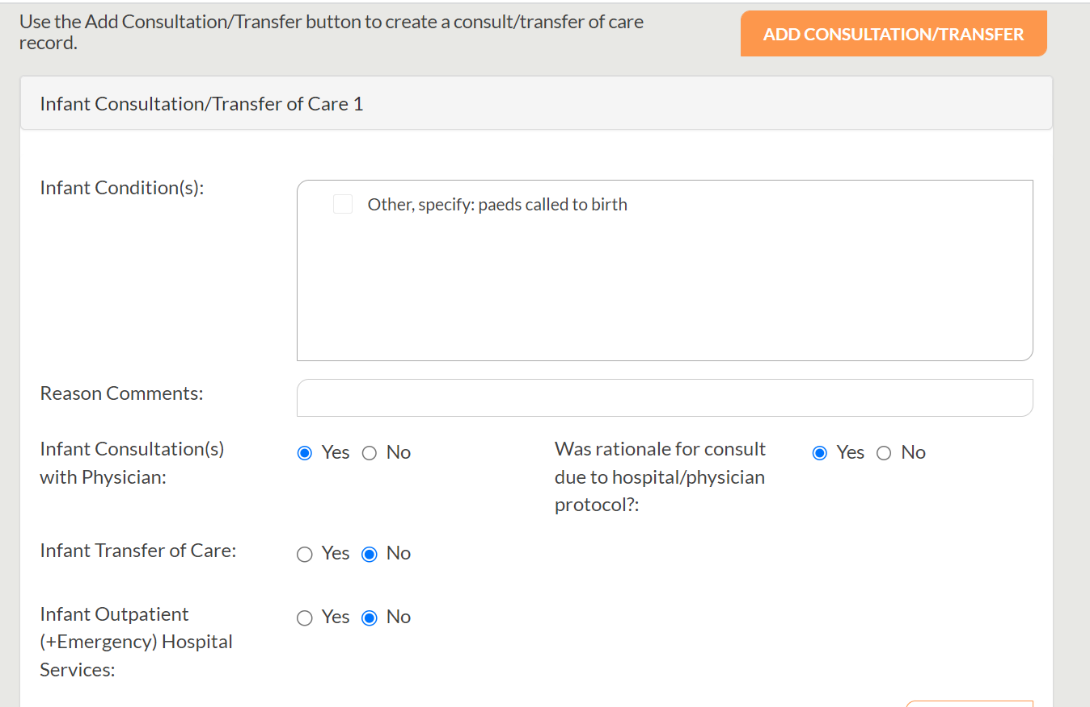
The above example describes a scenario in which a consultation is occurring only because the hospital protocol requires it to, not because the physician’s expertise was needed to attend to a clinical complication. Therefore, by selecting “Yes” for “Was rationale for consult due to hospital/physician protocol?” it clarifies that this consultation only occurred because of hospital/physician protocol. To learn more about this new data element read the response to the question “What does the question ‘Was rationale for consult/TOC due to hospital/physician protocol?’ intend to capture?” below.
When is it appropriate to record a consultation for an epidural during labour?
Although the BIS requires midwives to record all consultations with physicians during a course of care, a consultation during labour with an anesthetist for a routine epidural does not typically need to be recorded as a consultation.
If an anesthetist is called to place an epidural for a client during labour but there is no involvement of any other physician in this process, then the epidural would not be considered a reason for a consultation. This will be the case for most routine epidurals where the client does not have a clinical condition or complication of complex, obscure, or serious nature.
If a midwife is required by their hospital to first consult with an obstetrician or a physician other than the anesthetist to access an epidural during labour for a client (either due to hospital protocol and/or due to the complex, obscure or serious nature of the client’s condition), then the epidural would be considered a reason for a consultation.
- When hospital protocol requires a consultation/TOC to access an epidural: In this case, the midwife would not have required the involvement of a physician other than the anesthetist to provide the client with the epidural, but the hospital protocol requires that an additional physician is involved. To record this consultation/TOC, select “Pain Management-Epidural” as the reason for the consultation/TOC, and select “Yes” for “Was rationale for consult due to hospital/physician protocol”.
- When a client has a clinical condition that is complex, obscure, or serious in nature and consultation/TOC is needed to access an epidural: In this case the care/knowledge of a physician other than the anesthetist is required before an epidural can be administered and the care/knowledge provided by this physician is not within the knowledge, skills and/or judgement of the midwife. To record this consultation/TOC, select “Pain Management-Epidural” as the reason for the consultation/TOC, and select “No” for “Was rationale for consult due to hospital/physician protocol”.
If further context is needed to describe why the epidural was administered and/or why a consult was needed to access the epidural, these details can be added in the “Reason Comments” comment box. For example, epidural may be administered to manage blood pressure concerns; therefore, the comment “Epidural to manage blood pressure” can be added to this comment box.
If a client goes to a hospital emergency department in the antenatal period, does the midwife need to record this as a consultation?
If the midwife did not consult directly with a physician at the hospital, this would not be recorded as a consultation.
Midwives should only record their client’s visit with another care provider as a consultation/TOC if all the below items are met:
- the care provider being consulted with/transferred to is a physician,
- the clinical concern being addressed is related to/impacting the current pregnancy, birth, postpartum and/or neonate(s), and
- the midwife is in communication with the physician and is requesting the advice of the physician after each visit.
The clinical indication that necessitated the hospital visit may be captured under health conditions or pregnancy complications (or other appropriate fields).
If a client requires specialist appointments with a physician (for obstetric concerns or non-obstetric concerns) are these recorded in the BIS?
Midwives should record their client’s appointment with a specialist as a consultation/TOC if all the below items are met:
- the care provider being consulted with/transferred to is a physician,
- the clinical concern being addressed is related to/impacting the current pregnancy, birth, postpartum and/or neonate(s), and
- the midwife is in communication with the physician and is requesting the advice of the physician after each visit.
For example, if the midwife is the most responsible provider (MRP) and their client sees a psychiatrist regularly during the antenatal period for management of their mental health and the midwife is requesting advice after every visit from the physician, then the visits with the psychiatrist meet the definition of a consultation. The midwife would only need to record one consultation in the Antenatal General Encounter in the BIS to account for these appointments, even if there are several, so long as all the appointments address the same clinical complication.
If the complication worsens/changes and more specialist care is required than midwifery care, then the midwife/client/specialists can agree that it’s better to transfer care to a specialist (and the midwife can remain in a supportive role) and the specialist becomes the MRP for the client. There can only ever be one MRP at any given time for a client. This would then be recorded in the BIS as a transfer of care.
However, if in this same scenario, the midwife is not requesting the advice of the psychiatrist at every visit, then the visits with the specialist do not meet the definition of a consultation. The care from the specialist may be considered and care may be adjusted in response to changes created by the pregnancy, but the midwife would still be managing overall antenatal care. No consultation would be recorded in the BIS.
Non-obstetrical appointments with a physician that are not related to or impacted by the client’s pregnancy, such as a visit with an optometrist for a new eyeglass prescription, should not be recorded in the BIS.
What to Input for Additional Fields
What do I input into the “Reason Comments” box when I record a consultation/TOC?
When recording a consultation/TOC a “Reason Comments” box appears. This box is intended to capture clinically relevant information/context about the reason for a consultation/TOC. See the screenshot below for an example of an appropriate comment that can be left in this field.
If BORN sees a repeated pattern of information entered in “Reason Comments” box, it may prompt them to include a new data entry field. However, midwives are not required to enter anything into this comment box and in most cases should leave this field blank. Midwives should take care to not include any private or personal information about their client in the comment box.
If a client goes to an emergency room and receives treatment for a clinical indication, is this “Outpatient (+Emergency) Services = Yes”, and “Admission to Hospital = Yes”?
Firstly, this emergency visit should only be recorded as a consultation/TOC if the midwife directly consulted with the physician that provided the client care in hospital.
Midwives should only record their client’s visit with another care provider as a consultation/TOC if all the below items are met:
- the care provider being consulted with/transferred to is a physician,
- the clinical concern being addressed is related to/impacting the current pregnancy, birth, postpartum and/or neonate(s), and
- the midwife is in communication with the physician and is requesting the advice of the physician after each visit.
A client that visits an emergency room will likely receive outpatient care only, meaning they are provided care in the hospital but are not admitted into a room to stay overnight at the hospital. If a client received outpatient care at a hospital and the midwife did not communicate directly with the physician that provided care, then this should not be recorded in the BIS.
If a client received outpatient care at a hospital and the midwife did communicate directly with the physician that provided care, then this should be recorded as a consultation in the BIS. For “Antenatal Outpatient (+Emergency) Services” select “Yes”; for “Antenatal Admission to Hospital in Pregnancy” select “No”.
If a client visits an emergency room and is formally admitted to the hospital (i.e., given access to a room/bed to stay for one or more nights to receive treatment), then this would be considered a transfer of care. A midwife would record this as “Antenatal Outpatient (+Emergency) Services” select “Yes”; for “Antenatal Admission to Hospital in Pregnancy” select “Yes”. The client’s care is transferred to the responsible physician at the hospital for the duration of the client’s stay and transferred back to the midwife upon discharge from the hospital.
If a client visits the hospital for a scheduled, non-emergency appointment with an obstetrician during their regular clinic hours (i.e. the OB’s antenatal clinic is in the hospital), is this consultation considered an “Antenatal Outpatient (+Emergency) Service” in the BIS?
As a recent update to the BIS in December 2025, the data element “Antenatal Outpatient (+Emergency) Service” was renamed to improve clarity to: “Antenatal Unscheduled Emergency/Urgent Visits to the Hospital”. This data element intends to capture the use of unscheduled emergency/urgent triage visits to hospital.
The label help for previous version of the data element appeared as:
The label help for the new version of the data element appears as:
This change was in response to confusion in cases where an obstetrician’s antenatal clinic is located within a hospital. Scheduled, non-emergency clinic visits that happen to be in a hospital should not be captured with this data element. Please indicate “No” for “Antenatal Unscheduled Emergency/Urgent Visits to Hospital”, and “No” for “Antenatal-Admission to hospital in pregnancy”.
The same logic also applies to the “‘Infant Unscheduled Emergency/Urgent Visits to Hospital” data element in the Birth Child Encounter. Only indicate “Yes” to this data element if the infant required unscheduled emergency/urgent services in hospital.
What does the question “Was rationale for consult/TOC due to hospital/physician protocol?” intend to capture?
The question “Was rationale for consult due to hospital/physician protocol?” is a recent 2021 addition to the BIS as recommended by the AOM. A midwife may choose to go forward with a consultation/TOC for several reasons including because:
- It was within their clinical discretion to do so (considering their knowledge, skills, and judgement)
- It was the client’s preference, and this was supported by the midwife
- It was required by hospital/physician protocol
In the AOM’s recommendation to BORN, we explained that midwives would benefit from being able to differentiate between consultations/TOC that occurred because they were within a midwife’s clinical discretion and those that occurred because the hospital/physician required them (i.e., the midwife would not have chosen this option otherwise). This way there would be data to review how often midwives are essentially being forced to consult/transfer care due to hospital/physician policy. For the future 2023 BIS update, the AOM has recommended to BORN to include more of this context in the data description of this new data element to improve clarity.
This new data element also replaces a former data element entitled: “What was the rationale for this consultation/transfer of care?”, with the responses including: hospital protocol, college protocol, midwife discretion, and parental discretion. This data element was removed because midwives expressed to the AOM that they were often unsure which option to select since several responses could be relevant. The BORN KT Task Force also felt that this data element did not provide midwives with useful data to extract from the BIS about why consultations/TOC were occurring.
Answering this Data Element
Consider if the rationale for this consultation/TOC is ONLY due to hospital/physician protocol and if the clinical complication could have been managed by you within your current knowledge, skills, and judgment. If so, select “yes”.
If the rationale for this consultation/TOC was within your clinical discretion (i.e., the clinical complication is outside your current knowledge, skills and/or judgment and/or you approved of the client’s choice to involve a physician in their care), select “no”.
BORN used to ask about the rationale for a consultation/TOC with options for response including hospital protocol, college protocol, midwife discretion, and parental discretion. Where did this question go?
At the request of the AOM, this question was removed during the 2021 update of the BIS and was replaced with the question: “Was rationale for consult due to hospital/physician protocol?”. To learn more about this new data element, read the above response to the question: “What does the question ‘Was rationale for consult/TOC due to hospital/physician protocol?’ intend to capture?”.
The data element “What was the rationale for this consultation/transfer of care?” was removed because midwives expressed to the AOM that they were often unsure what to select since several responses could be relevant. The BORN KT Task Force also felt that this data element did not provide midwives with useful data to extract from the BIS about why consultations/TOC were occurring.
Scope of Practice
How do I determine my scope of practice now that the consultations/TOC standard has been rescinded by the CMO?
Midwives must assess their own knowledge, skills, and judgement to provide care within the legislative scope of practice. This scope of practice may vary from midwife to midwife based on factors such as experience, training, and practice settings. Midwives should refer to the CMO's Scope of Practice document (PDF, 1 MB) (along with its included decision tree (PDF, 207 KB)) and the AOM’s FAQ on Scope of Practice to understand what is changing and what it might mean for their scope of practice now and in the future.
How do I record consultations/TOC that may be considered shared care with a physician?
Although there are circumstances in which a midwife and a physician may engage in collaborative care, the CMO no longer acknowledges the concept of “shared care”. At any given time, there can only be one most responsible care provider (MRP), and thus care cannot be equally “shared” amongst a midwife and a physician.
If the midwife remains the MRP but is involving a physician to collaborate in a client’s care by seeking guidance or support on a particular concern, this is a consultation.
If the physician becomes the MRP (i.e., is now primarily responsible for managing the client’s care), and the midwife continues collaborating on certain aspects of care that are within midwifery scope, this a transfer of care.
For more information on scope of practice as it relates to consultations/TOC review the AOM's FAQ on Scope of Practice.