#MidwiferyDataMatters: What is the true demand for midwifery care?

January 14, 2026
The demand for midwifery care in Ontario continues to outpace the supply—but by how much?
In the AOM’s commitment to improving the sustainability of the midwifery profession, this question has been of utmost importance. The Roadmap to Health System Integration reports that between 2013-2022, “over 22,000 clients were unable to access the midwifery care they sought,” citing BORN Ontario. This same number is emphasized again in the visual summary (see graphic below), but the footnote beneath the graphic states that a larger story is being left untold.
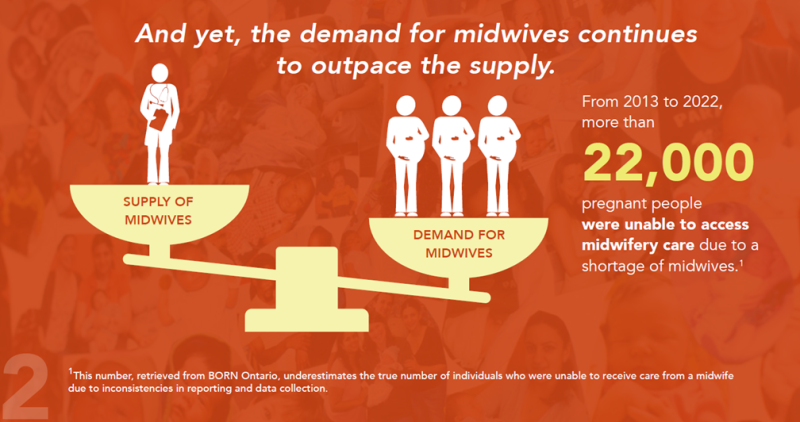
The reality: 22,000 is likely a gross underestimation of the true number of people on midwifery waitlists from 2013-2022, and incomplete data entry submitted to BORN is the suspected cause.
The problem with unaccommodated client data
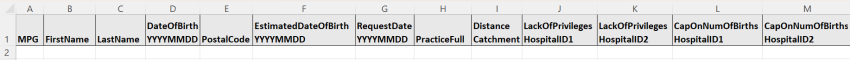
When a potential client contacts a practice group seeking midwifery care, but care is unavailable, they are added to a waitlist. If care cannot be accommodated for this individual due to lack of availability of midwifery services, they are then considered unaccommodated and should be recorded as such under the Unaccommodated Client Data (UCD) system in the BORN Information System (BIS). MPGs are required to enter UCD data as part of the MPG-TPA agreement and submit their Schedule J report in the BORN Information System (BIS) by the 15th day after each quarter of the fiscal year (due dates for each quarter: July 15, October 15, January 15, and April 15).
From 2012 to the current day, there continues to be inconsistencies with MPG reporting of UCD data. To track where a waitlisted client ultimately received care, BORN needs to be able to match the information gathered from the waitlist of the MPG to an existing entry within the BIS. When UCD is entered correctly, BORN can effectively match the client's information and find out where the client ultimately received care. Unfortunately, the process of accurately matching is complicated when data entry has:
- inaccurate/incomplete client name information, such as only initials, or a pseudonym (e.g. Jane Doe)
- inaccurate postal code information, such as entering the MPG’s postal code in place of the client’s and/or
- missing information crucial for matching, such as the client’s date of birth.
The resulting data set from 2013-2022 can then be divided into three buckets:
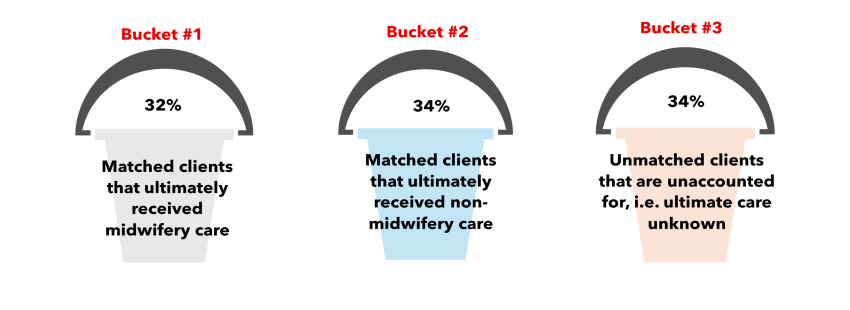
From 2013-2022, 34% clients who initially requested and were denied midwifery care were unaccounted for in the BIS.
Revisiting the “22,000 clients” mentioned above that requested but did not ultimately receive midwifery care, this number refers to clients in bucket #2, i.e. matched clients that we know ultimately received non-midwifery care. It is highly likely that a significant portion of unmatched clients in bucket #3 belong in bucket #2, thus why the true extent of the demand for midwifery services remains unknown.
This problem persists with more recent data. From 2023-20241, of the clients who requested midwifery care and were put on the waitlist:
- over 6600 (38%) ultimately received non-midwifery care
- over 4700 (27%) ultimately received midwifery care, and for
- over 6000 (35%) the ultimate care is unknown.
Moving forward: Data entry tips
Strategies at BORN
BORN introduced various system improvements in the Fall of 2024 including:
- moved UCD data entry from the Midwifery Invoicing System (MIS) to the BIS
- streamlined reasons for not accommodating at MPG
- search and filter functions
BORN is in the process of launching new and updated resources (1 updated guide and 1 new FAQ) to support accurate data entry that will be available in the BIS Help Section under “BORN Reference Guides and Training Materials.” Once available, announcement of these resources will be provided in the AOM’s Midwifery Memo and through BORN’s communication team. Among the existing resources is a fillable spreadsheet that indicates the exact information needed for accurate and complete data entry and allows an entire list of UCD to be uploaded to the BIS all at once, eliminating the need for manual data entry for each waitlisted client. This spreadsheet is available in the BIS Help section and is also on the AOM website for download under "NEW! Unaccommodated Client Data (UCD)" on this member's only page (login required).
Strategies for MPGs
To support the ongoing effort to improve UCD data quality, MPGs should ensure that intake form templates are reviewed and updated to collect full and accurate information on the following items about clients requesting care:
- First name
- Last name
- Client date of birth
- Postal code
- Estimated date of birth
- Request date
In some cases, MPGs may be entering incomplete data for the above fields due to potential clients indicating that they “do not consent” to share their information with BORN. However, BORN does not require consent to collect Personal Health Information (PHI) from MPGs. BORN is a prescribed registry under the Personal Health Information Protection Act (PHIPA) and as such has additional privacy and information security controls for storing data containing PHI. Further, BORN conducted an extensive internal review to confirm this, including consultation with the Ontario Midwifery Program. MPGs should remove any questions on their intake form pertaining to gathering consent to share PHI with BORN as it is unnecessary and misleading for potential clients. This information was recently circulated to MPGs in a notice from BORN.
Client consent is not needed to report UCD to BORN. MPGs are not required to ask clients on their intake form if they consent to sharing this information with BORN.
MPGs should also familiarize themselves with the reasons a client could not be accommodated at an MPG. BORN provides the following categories:
- practice full (no capacity to take on new clients due to no more caseload or not enough midwives)
- distance catchment – no transportation
- hospital integration issue – lack of privileges
- hospital integration issue – cap on number of births
More detailed information on these categories will be available in the upcoming BIS Help Section resources.
Importantly, MPGs should understand that not all waitlisted clients are considered unaccommodated. Waitlisted clients that experience miscarriage/abortion prior to being offered midwifery care and those unaccommodated due to practice decisions, such as repeat cesarean birth, twins or other situations within midwifery scope, should not be captured in the UCD system.
Making use of UCD
Advocacy efforts
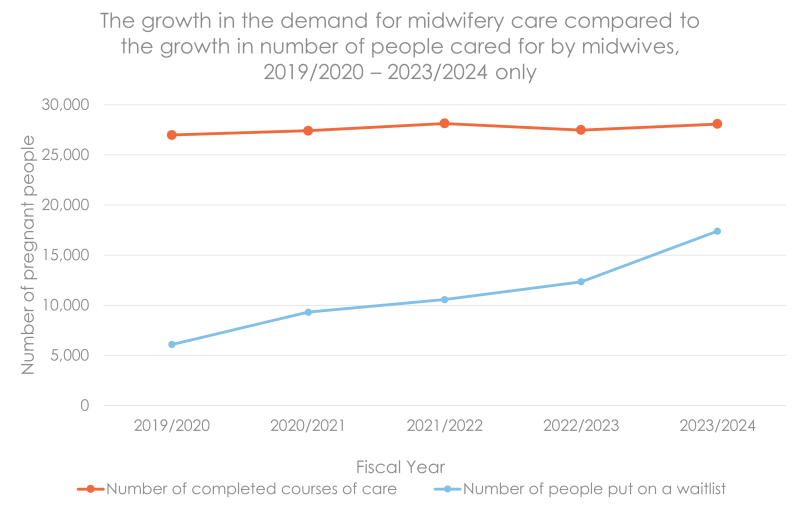
The growth in demand for midwifery services over time is evident. From the 2019-2020 to 2023-2024 fiscal year, the number of clients midwives cared for increased by only 1090 people (from 26 983 to 28 073). In the same years, the number of pregnant people requesting midwifery care and initially being put on a waitlist due to practice being full grew by 11 309 people (from 6083 to 17 392), almost tripling over that time. The increasing demand for midwifery care is far outpacing the growth in midwives’ capacity to provide care (see graph below).
The AOM uses this data in negotiations, emphasizing the need for midwifery growth and identifying target areas where expansion and funding is needed most.
Expanding access to midwifery services
Locally, this data can support midwives in efforts to expand services. For example, Hawthorne Midwives utilized UCD as part of an evidence-based campaign demonstrating a gap in the current health-care system to attend to underserved communities, ultimately increasing midwifery staffing and caseload funding.
Moving forward, with a concerted and collaborative effort for consistent data entry, midwives can feel more confident that the UCD collected in BORN is truly representative of the demand for midwifery care. This data supports the AOM’s calls to action to improve the sustainability of the midwifery profession and increase access to care.
Want to learn more? Register now for our upcoming webinar at 12 p.m. on Jan. 21, 2026: Tracking demand for midwifery services: Unaccommodated Client Data in the BORN Information System.
1. Better Outcomes Registry and Network (BORN) Ontario. Years Provided: (2013 to 2025). Resource Type: Tabulated data. Data Extracted on 7 Aug, 2025.