Safe Medication Practice
As primary care providers, midwives diagnose and prescribe according to their scope of practice, and according to their own knowledge, skill and judgement. In 2024, Ontario Regulation 188/24: Designated Drugs and Substances, under the Midwifery Act, 1991 was updated and expanded.
- The College of Midwives of Ontario (CMO) has created a resource page outlining what’s new in the regulation.
- The AOM has a FAQ on preparing to prescribe or administer drugs that are new to midwives. The now rescinded practice standard regarding Prescribing and Administering Drugs, October 2019 (PDF, 104 KB) may also be helpful.
Medication safety is complex and multifactorial. It requires clear collaboration and communication between client, providers and community pharmacy, and an open, proactive approach to addressing no harm, near miss and harmful safety incidents. Health Quality Ontario suggests “organizations support a patient safety culture that is person-centered, just and trusting ” (PDF 491 KB). The AOM has various resources on just culture, adverse events, critical incidents reviews and disclosure. Any medication error should be reported to both HIROC and the Institute for Safe Medication Practice Canada (ISMP). The ISMP reporting process is straightforward, and can be anonymous. Reporting incidents can help researchers and policy makers recommend systems level changes to packaging and processes to prevent errors in future.
Midwives who undertake education or training on expanded pharmacopeia or on safe medication practices should keep a log of any hours, courses and clinical experience. AOM OnCall is available for support related to quality and risk management.
Safe prescribing
Prescribing medications can improve health outcomes, quality of life and client experience. However, any medication also has the potential to cause harm. The following general principles apply:
- Remain familiar with the CMO standards in addition to any local practice/clinic/hospital policies or procedures.
- Maintain and develop your pharmacology knowledge and identify professional practice resources and clinical tools to support you in your learning and practice.
- Consider whether you have sufficient information to prescribe safely:
- Identify and address language or communication barriers to obtaining a client’s health or medication history and understanding their concerns, ideas and priorities.
- Create and revisit each client’s best possible medication history, including any over the counter medications and supplements.
- Take into account whether any physical assessments may be necessary, and the mode of consultation you are using (virtual or in person).
- Utlilize electronic systems or documentation strategies which improve safety, such as an EMR which flags medication interactions or allergies and/or electronic prescriptions, which reduce errors due to legibility. If using written prescription pads, ensure they are personalized and numbered.
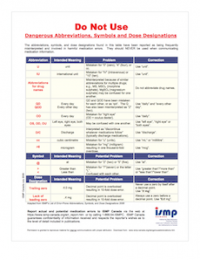
- Consider your abbreviations and dose designations carefully. ISMP Canada has developed a Dangerous Abbreviations, Symbols and Dose Designation list. This list was recently updated (2025) by ISMP Canada and identifies abbreviations and symbols associated with harm or potential for harm.
- Develop and document a plan for monitoring for therapeutic or adverse effects with the client and adjusting dosages as needed.
- Document in the client’s chart and report any adverse effects of the medication. Consult as necessary with another health care provider if the drug therapy causes an unanticipated response.
- If a medication is ordered by another healthcare provider, ensure timely communication of the client’s response to the drug with the prescriber.
- Ensure the client has a plan for continuing care and monitoring of any medications which will continue after discharge from midwifery care.
While midwives report few medication errors, HIROC notes those that are reported reflect similar trends. Midwives should consider developing a protocol to avoid the risk of adverse drug events by referring to the College’s now rescinded standard on Prescribing and Administering Drugs and their hospital’s policies.
Medication administration
From 2015 to 2020, 7531 harmful medication incidents were voluntarily reported to the ISMP Canada and the Canadian Institute for Health Information’s National System for Incident Reporting (ISMP Canada Safety Bulletin, Vol 20(11) Dec 22, 2020, PDF 2.3 MB). ISMP Canada reported that 86% of these incidents resulted in mild harm. Medications that are most frequently reported in harm incidents across all healthcare settings include morphine and acetaminophen. In obstetrical care, the most common errors relate to oxytocin incidents (PDF 497 KB).
Various strategies can be adopted by individuals and organizations to mitigate client safety risks related to medication administration.
Low Tech Strategies
• using the 10 rights of medication administration (HIROC, Risk Profile – Medication Adverse Events);
• allergy armbands;
• implementing independent double checks (i.e., another midwife to verify the drug, concentration, dose and route) for drugs with higher risk of adverse outcomes in the event of an error;
• minimizing interruptions during medication preparation and administration;
• clear hand-offs at transitions of care;
• safe, standardized storage and handling of medication according to the manufacturer’s recommendations (e.g., stored separately from specimens, monitoring expiry dates); Refer to the AOM's Template Refrigerator Policy for details (under Infection Prevention & Control);
• following public health and blood bank guidelines when disposing of unused or expired products; and
• labeling medications and IV solutions in all settings using consistent, legible labels.
High Tech Strategies
• Allergy documentation and alerts in electronic medical record and pharmacy system;
• pre-use and in-use oxytocin safety checklists;
• interaction alerts in EMRs; and
• smart infusion pumps for IV infusions.
Practice resources
Bugs & Drugs: website | Google Play Store | Apple App Store A peer-reviewed, evidence based antimicrobial reference guide for management of infectious diseases and appropriate antimicrobial use. A specific section on infections in pregnancy exists and it is frequently updated. Bugs & Drugs is supported by the Antibiotic Wise program and is funded in BC by the BC Ministry of Health.
Clinical Practice Guidelines & Clinical Treatment Algorithms Developed by the Clinical Knowledge Translation team at the Association of Ontario Midwives.
Drugs Rx App: Google Play Store App | Apple App Store Updated on a regular basis by the Clinical Knowledge Translation team at the Association of Ontario Midwives.
Drugs and Lactation Database (LactMed), National Library of Medicine
Drug Product Database, Health Canada
e-lactancia is a project from the Association for Promotion of and Cultural and Scientific Research into Breastfeeding
ISMP Canada Safety Bulletins: subscribe and learn about strategies to mitigate harm and prevent medication errors. Audio briefs and PDFs available.
Licensed Natural Health Products Database (LNHPD), Government of Canada
Clinic posters
ISMP: 5 Questions to Ask (French)
Canadian Association of Midwives: "We can talk about it." (English | Indigenous)
These posters are directed at clients, prompting them to ask questions about their medications and vaccines. They can be posted in your waiting room or in clinic rooms.
Further education
ISMP Best Possible Medication History Interview Guide, (PDF 4.5 MB)
World Health Organization’s 1994 Guide to Good Prescribing: A Practical Manual (PDF 315 KB) lays out a six step framework for prescribing which continues to be used today in medical education.
Webinars:
Safe Prescribing in Everyday Practice: A refresher for midwives, 2025
Clinical reasoning: Differential diagnoses in midwifery care, 2025
Narcotics
Midwives who have undergone narcotic specific, additional training may now prescribe and administer the following opioid analgesics for in-hospital intrapartum pain management from a hospital pharmacy: meperidine, morphine sulfate, nalbuphine and fentanyl citrate. An eLearning module is available from the CMO, and midwives may wish to complement this with further learning in relation to the effectiveness of opioids for labour pain.
References
Errors Associated with Oxytocin Use: A Multi-Incident Analysis. ISMP Canada Safety Bulletin – Volume 19, Issue 8. October 23, 2019. See: https://ismpcanada.ca/wp-content/uploads/ISMPCSB2019-i8-Oxytocin.pdf
Medication Administration Errors. Paul MacDowell, PharmD, BCPS, Ann Cabri, PharmD, and Michaela Davis, MSN, RN, CNS. Patient Safety Network. Agency for Healthcare Research and Quality. March 12, 2021. See: https://psnet.ahrq.gov/primer/medication-administration-errors
Medication Errors and Adverse Drug Events. Patient Safety Network. Agency for Healthcare Research and Quality. September 7, 2019. See: https://psnet.ahrq.gov/primer/medication-errors-and-adverse-drug-events
Medication Safety; Care in all settings. Ontario Health Quality Standards. 2021. See: https://hqontario.ca/Portals/0/documents/evidence/quality-standards/qs-medication-safety-quality-standard-en.pdf
Ten Principles of Good Prescribing. British Pharmalogical Society. See: https://www.bps.ac.uk/getmedia/230ff608-3b47-4aa8-8659-c84d3e2906be/Clinical-Prescribing-Principles.pdf.aspx?ext=.pdf