That said, the specialized education and training that midwives undergo significantly contributes to the safety of birth centre births in Ontario.
Midwives:
- are regulated health professionals In Ontario, regulated health professions are governed under the Regulated Health Professions Act, 1991 (RHPA) and health profession Acts (i.e., Medicine Act, 1991). This legislative framework establishes health regulatory colleges, which regulate the professions in the public interest. Health regulatory colleges are responsible for ensuring that regulated health professionals provide health services in a safe, professional and ethical manner. This includes, among other things, setting standards of practice for the profession and investigating complaints about members of the profession and, where appropriate, disciplining them.1
The regulatory college for Ontario midwives is the College of Midwives of Ontario. Ontario Ministry of Health and Long Term Care. Regulated Health Professions [Internet]. Canada: Web; 1991.
- receive an education specific to attending births and responding to birth emergencies both in and outside of the hospital
- engage in regular, continuing competency training “Continuing competency training” refers to the minimum ongoing professional training the College of Midwives of Ontario requires of midwives in order to provide safe, responsible care throughout their career. For example, midwives must provide proof of certification in: Neonatal Resuscitation every year Emergency Skills Management every two years Cardio Pulmonary Resuscitation every two years to attend births and respond to birth emergencies both in and outside the hospital
- can quickly access specialist care (e.g. obstetrician, pediatrician) in the hospital when needed to support the best health outcomes for you and your baby
Over 2000 babies have been born safely at the Toronto and Ottawa birth centres since they opened their doors in 2014.
What does Canadian research say about the safety of planned free-standing birth centre births?
Midwife-led birth centres are somewhat new in Canada; however, they have long existed in the United Kingdom, Australia and the United States. Health outcomes at Ontario’s birth centres are being carefully tracked, but the birth numbers are still too low to make research-based conclusions.
A preliminary 2016 evaluationThe EVALUATION OF ONTARIO’S BIRTH CENTRE DEMONSTRATION PROJECT (Final Report: March 31, 2016) concluded that "care was low in intervention, safe (minimal negative outcomes and a transport rate comparable to the literature), well-integrated into the maternal-child health system, and satisfactory to women" and that "data collected from the BCs during the demonstration project supports the BC as a safe and effective option for women with low risk pregnancies seeking a low-intervention approach to their labour and birth."1Sprague AE, Sidney D, Darling EK, Van Wagner V, Soderstrom B, Rogers J, et al. Outcomes for the First Year of Ontario’s Birth Center Demonstration Project. J Midwifery Womens Health [Internet]. 2018 Sep;63(5):532–40. of the Ottawa and Toronto birth centres completed by Ontario’s Better Outcomes Registry and Network (BORN OntarioThe Better Outcomes Registry & Network (BORN) is Ontario's prescribed maternal, newborn and child registry with the role of facilitating quality care for families across the province. BORN collects, interprets, shares and rigorously protects high-quality data essential to making Ontario the safest place in the world to have a baby.Ontario B. About BORN [Internet]. [cited 2020 Jul 30].) concluded that:
- birth centres appear to safely support uncomplicated, low intervention births
- the vast majority of families who use birth centres were very satisfied with their experience and would choose to give birth there again
These conclusions are consistent with Canadian research that shows excellent health outcomes associated with midwife-attended home births. Home births and birth centre births have many important aspects in common including:
- midwives as the primary health care providers
- availability of similar medical equipment and medications
- availability of similar pain relief options
Because of these similarities, we can assume birth centre health outcomes are comparable to home birth health outcomes.
What does international research say about the safety of planned, free-standing birth centre births?
While there are no Canadian studies on the safety of midwife-attended birth centre births, international research provides insight into the issue.
In the United Kingdom (UK), over 15, 000 babies are born annually in free-standing midwifery units (FMUs). UK midwives practice in much the same way as Ontario midwives, and FMUs can be considered the UK equivalent of Ontario’s birth centres. Strong research from the UK shows excellent health outcomes for low risk birthing parents and their babies following planned FMU births.
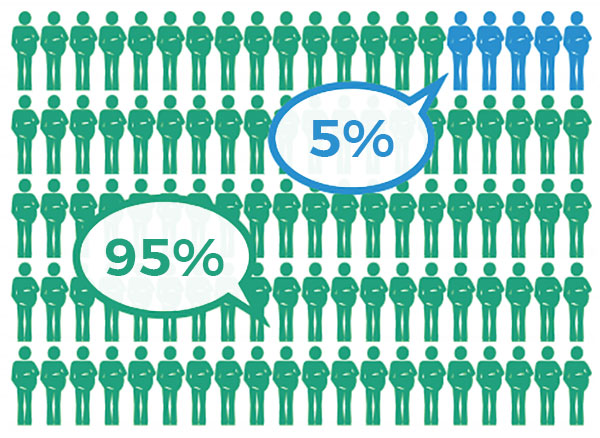
Infant outcomes by planned place of birth: obstetric unit (hospital) vs. free-standing midwifery unit (birth centre)
The diagrams* below show outcomes for babies when birth is planned in a hospital obstetric unit or an FMU (birth centre). In each case, the green circles represent a baby born healthy, and the blue circles represent a baby with a poor outcome (e.g., the baby was injured, seriously ill or died during or just after birth). These outcomes are very rare amongst healthy people who are at low risk of complications, but they can happen in any birth setting.
UK research indicates that the same number of babies are born healthy and well regardless of planned birth setting (FMU or obstetric unit).


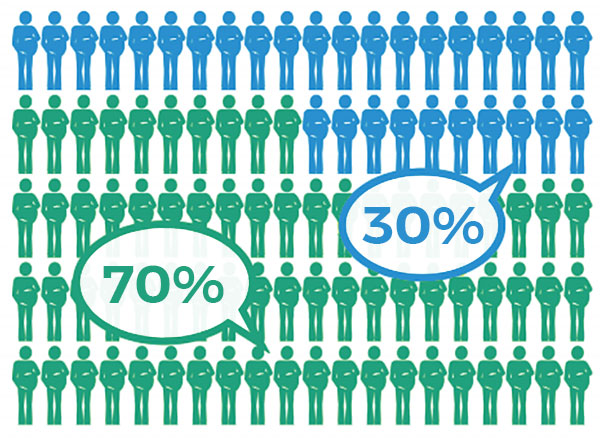
 birthing people who had an uncomplicated birth, free of interventions
birthing people who had an uncomplicated birth, free of interventions birthing people who experience interventions (induction of labour, birth assisted by instruments such as forceps and vacuum, c/sections, epidural, spinal or general anesthesia)
birthing people who experience interventions (induction of labour, birth assisted by instruments such as forceps and vacuum, c/sections, epidural, spinal or general anesthesia)